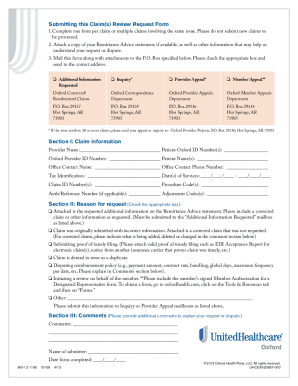
Resubmit claims in the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In > Claims & Payments. Your patient's plan may include a pre-notification requirement for services, including hospitalizations, other inpatient care, inpatient surgeries or surgical procedures and outpatient IV infusion therapy, radiation therapy and cardiac surgery. The following date stamps may be used to determine date of receipt: Note: Date stamps from other health benefit plans or insurance companies are not valid received dates for timely filing determination. In Connecticut: Anthem Health Plans, Inc. have hearing loss, Community Care Network Region 1 (authorized), Community Care Network Region 2 (authorized), Community Care Network Region 3 (authorized), Community Care Network Region 4 (authorized), Unauthorized Emergent Care (unauthorized).  Submit a copy of the primary carriers EOB with the claim to Health Options within sixty (60) days of the date of the primary carriers EOB. 3 0 obj
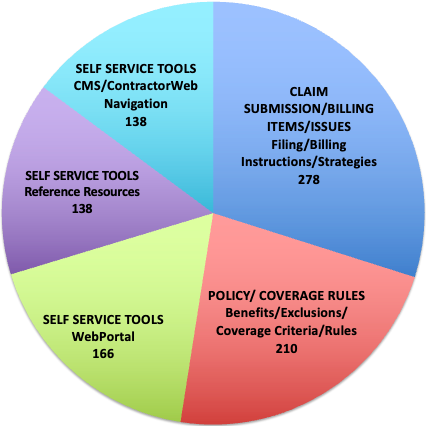
We also have to ask the claim received date for confirmation as well. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. WebBenefit Administration Company is a well-established, comprehensive employee benefit services provider. Do not resubmit claims that were either denied or pended for additional information using EDI or paper claims forms. WebICD-10. *%jXU E,Sbxw^t_o3rv&|w>%Q5T~xQOL'
\oM(14q`|4w^E{H(;S1{*w j;POnKYSr>)G9s". In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI), whichunderwrites or administersthe PPO and indemnity policies and underwrites the out of network benefits in POS policies offered by Compcare or WCIC; Compcare Health Services Insurance Corporation (Compcare) underwritesor administers the HMO policies and Wisconsin Collaborative Insurance Company (WCIC) underwrites or administers Well Priority HMO or POS policies. If you dont submit it within 45 days, you must submit an appeal with the information. Providers who submit original claims to Security Health Plan within appropriate timeframes can submit corrected claims or adjustment requests within Submit the requested information promptly as outlined in the request. You shall comply with the procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment. We handle billions of dollars in claims each year. If a claim is submitted past the filing deadline due to an unusual occurrence (e.g., health care provider illness, health care providers computer breakdown, fire, flood) and the health care provider has a historic pattern of timely submissions of claims, the health care provider may request reconsideration of the claim. If the claims and records do not conform to the minimum requirements for conversion to the 837 or 275 electronic formats, they are rejected and sent back for correction. Larger organisations use software that assist benefits administrators. Only covered services are included in the computation of the reinsurance threshold. Many members Know what services have a surcharge and bill those services accordingly. Hospital reimbursement: We reimburse hospitals for services provided to members at rates established in the attachment of the hospital contract. Complete and accurate standard Center for Medicare & Medicaid Services (CMS) or electronic transaction containing false claims notice (such as CMS 1450, CMS 1500 or 837 EDI transaction). You are required to submit to clean claims for reimbursement no later than 1) 90 days from the date of service, or 2) the time specified in your Agreement, or 3) the time frame specified in the state guidelines, whichever is greatest. If you do not submit clean claims within these time frames, we reserve the right to deny payment for the claim (s). Web240 - Time Limits for Filing Appeals & Good Cause for Extension of the Time Limit for Filing Appeals 240.1 - Good Cause 240.2 - Conditions and Examples That May Establish Make sure your out-of-area patients get covered for the care they need. 1703) 180 days: For CCN, submit to TriWest or Optum For VCA or local Release of information: Under the terms of HIPAA, we have the right to release to, or obtain information from, another organization to perform certain transaction sets. NOTE: The processes outlined below are exclusive to supplying documentation for unauthorized emergent care. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. The author and contributor of this blog N.K.Singh (NSingh) is working in Medical Billing and Coding since 2010. %PDF-1.7
You are strongly encouraged to electronically submit claims and required supporting documentation. For UnitedHealthcare West encounters, the Payer ID is 95958. To avoid the denial, charges must be created within 24 hours from the service date and has to be sent out to the payer on the same day.
Submit a copy of the primary carriers EOB with the claim to Health Options within sixty (60) days of the date of the primary carriers EOB. 3 0 obj
We also have to ask the claim received date for confirmation as well. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. WebBenefit Administration Company is a well-established, comprehensive employee benefit services provider. Do not resubmit claims that were either denied or pended for additional information using EDI or paper claims forms. WebICD-10. *%jXU E,Sbxw^t_o3rv&|w>%Q5T~xQOL'
\oM(14q`|4w^E{H(;S1{*w j;POnKYSr>)G9s". In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI), whichunderwrites or administersthe PPO and indemnity policies and underwrites the out of network benefits in POS policies offered by Compcare or WCIC; Compcare Health Services Insurance Corporation (Compcare) underwritesor administers the HMO policies and Wisconsin Collaborative Insurance Company (WCIC) underwrites or administers Well Priority HMO or POS policies. If you dont submit it within 45 days, you must submit an appeal with the information. Providers who submit original claims to Security Health Plan within appropriate timeframes can submit corrected claims or adjustment requests within Submit the requested information promptly as outlined in the request. You shall comply with the procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment. We handle billions of dollars in claims each year. If a claim is submitted past the filing deadline due to an unusual occurrence (e.g., health care provider illness, health care providers computer breakdown, fire, flood) and the health care provider has a historic pattern of timely submissions of claims, the health care provider may request reconsideration of the claim. If the claims and records do not conform to the minimum requirements for conversion to the 837 or 275 electronic formats, they are rejected and sent back for correction. Larger organisations use software that assist benefits administrators. Only covered services are included in the computation of the reinsurance threshold. Many members Know what services have a surcharge and bill those services accordingly. Hospital reimbursement: We reimburse hospitals for services provided to members at rates established in the attachment of the hospital contract. Complete and accurate standard Center for Medicare & Medicaid Services (CMS) or electronic transaction containing false claims notice (such as CMS 1450, CMS 1500 or 837 EDI transaction). You are required to submit to clean claims for reimbursement no later than 1) 90 days from the date of service, or 2) the time specified in your Agreement, or 3) the time frame specified in the state guidelines, whichever is greatest. If you do not submit clean claims within these time frames, we reserve the right to deny payment for the claim (s). Web240 - Time Limits for Filing Appeals & Good Cause for Extension of the Time Limit for Filing Appeals 240.1 - Good Cause 240.2 - Conditions and Examples That May Establish Make sure your out-of-area patients get covered for the care they need. 1703) 180 days: For CCN, submit to TriWest or Optum For VCA or local Release of information: Under the terms of HIPAA, we have the right to release to, or obtain information from, another organization to perform certain transaction sets. NOTE: The processes outlined below are exclusive to supplying documentation for unauthorized emergent care. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. The author and contributor of this blog N.K.Singh (NSingh) is working in Medical Billing and Coding since 2010. %PDF-1.7
You are strongly encouraged to electronically submit claims and required supporting documentation. For UnitedHealthcare West encounters, the Payer ID is 95958. To avoid the denial, charges must be created within 24 hours from the service date and has to be sent out to the payer on the same day.  Other Health Insurance (OHI) and Explanation of Benefits (EOBs), Any other document type normally sent via paper in support of a Veteran unauthorized emergency claim. VA is also the primary and sole payer for unauthorized emergent care approved under 38 U.S.C.
Other Health Insurance (OHI) and Explanation of Benefits (EOBs), Any other document type normally sent via paper in support of a Veteran unauthorized emergency claim. VA is also the primary and sole payer for unauthorized emergent care approved under 38 U.S.C. 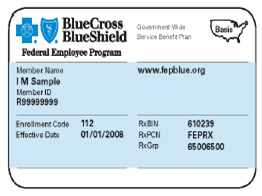 For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. In Maine: Anthem Health Plans of Maine, Inc. We coordinate benefits for members who are Medicare beneficiaries according to federal Medicare program guidelines. Box 202117Florence SC 29502, Logistics Health, Inc.ATTN: VA CCN Claims328 Front St. S.La Crosse WI 54601, Secure Fax: 608-793-2143(Specify VA CCN on fax). Continue with Recommended Cookies, Medical Billing and Coding Information Guide. Administrative. An itemized bill is required to compute specific reinsurance calculations and to properly review reinsurance claims for covered services. The time limit starts from the date of service, when the medical procedure was performed, and ends on the date when the insurance company receives the claim. While VA always encourages providers to submit claims electronically, on and after May 1, 2020, it is important that all documentation submitted in support of a claim comply with one of the two paper submission processes described. For help using Availity, log onto Availity.com and select the Help & Training tab. <>/ExtGState<>/XObject<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/Annots[ 12 0 R 20 0 R 22 0 R 23 0 R 24 0 R 25 0 R 26 0 R 28 0 R 29 0 R 31 0 R 32 0 R 33 0 R 35 0 R 36 0 R 37 0 R 39 0 R 45 0 R 46 0 R 47 0 R 49 0 R 50 0 R 51 0 R 52 0 R 54 0 R 55 0 R 56 0 R 58 0 R 59 0 R 61 0 R 62 0 R 63 0 R 65 0 R 66 0 R 70 0 R 75 0 R 76 0 R 77 0 R 78 0 R] /MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S>>
Allied has two payer IDs. If you would like to verify insurance benefits, contact the benefit verification line: 866-323-2985. We have a track record of providing quality medical billing services to multiple healthcare organizations and specialty providers across USA.
For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. In Maine: Anthem Health Plans of Maine, Inc. We coordinate benefits for members who are Medicare beneficiaries according to federal Medicare program guidelines. Box 202117Florence SC 29502, Logistics Health, Inc.ATTN: VA CCN Claims328 Front St. S.La Crosse WI 54601, Secure Fax: 608-793-2143(Specify VA CCN on fax). Continue with Recommended Cookies, Medical Billing and Coding Information Guide. Administrative. An itemized bill is required to compute specific reinsurance calculations and to properly review reinsurance claims for covered services. The time limit starts from the date of service, when the medical procedure was performed, and ends on the date when the insurance company receives the claim. While VA always encourages providers to submit claims electronically, on and after May 1, 2020, it is important that all documentation submitted in support of a claim comply with one of the two paper submission processes described. For help using Availity, log onto Availity.com and select the Help & Training tab. <>/ExtGState<>/XObject<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/Annots[ 12 0 R 20 0 R 22 0 R 23 0 R 24 0 R 25 0 R 26 0 R 28 0 R 29 0 R 31 0 R 32 0 R 33 0 R 35 0 R 36 0 R 37 0 R 39 0 R 45 0 R 46 0 R 47 0 R 49 0 R 50 0 R 51 0 R 52 0 R 54 0 R 55 0 R 56 0 R 58 0 R 59 0 R 61 0 R 62 0 R 63 0 R 65 0 R 66 0 R 70 0 R 75 0 R 76 0 R 77 0 R 78 0 R] /MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S>>
Allied has two payer IDs. If you would like to verify insurance benefits, contact the benefit verification line: 866-323-2985. We have a track record of providing quality medical billing services to multiple healthcare organizations and specialty providers across USA. 
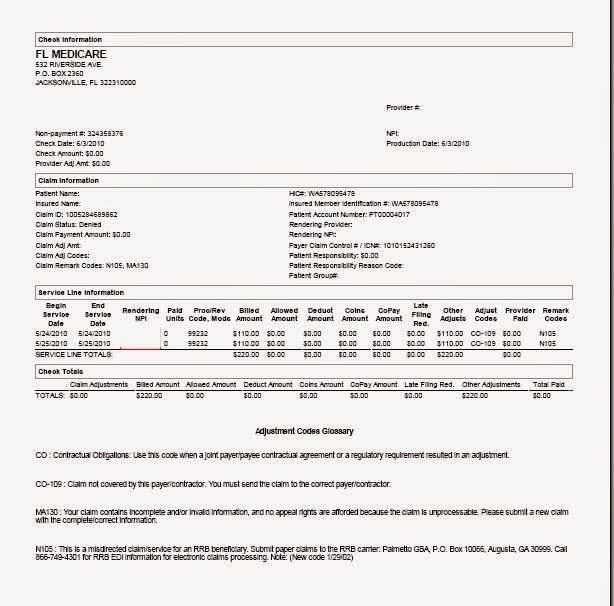 With the exception of supplying remittance advice supporting documentation for timely filing purposes, these processes do not apply to authorized care. When a claim is submitted to us as the primary payer, and we are the secondary payer, our claims system will deny the claim because we dont have the EOB. WebBenefits administration definition. Need access to the UnitedHealthcare Provider Portal? We have primary responsibility if any of the following apply to the member: Additional copies of EOBs/remittance advice: Should you misplace a remittance advice, you may obtain a copy by logging in to the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Find instructions and quick tips for EDI on uhcprovider.com/edi. Modifiers: Modified procedures are subject to review for appropriateness consistent with the guidelines outlined in our policies. hbbd``b`S$$X fm$q="AsX.`T301 WebExpert Administration Without the Waste. For complete details regarding the reimbursement of recognized modifiers, refer to the Modifier Reference policy at uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans. For institutional claims, include the billing provider National Uniform Claim Committee (NUCC) taxonomy. Try to keep all information in the latest update and will update as per receive any new information. If the billed level of care is at a higher level than the authorized level of care, we pay you the authorized level of care. If electronic capability is not available, providers can submit claims by mail or secure fax. Benefit Administration is the process of creating, managing and updating an organizations employee benefits program. Community providers should remain in contact with the referring VA Medical Center to ensure proper care coordination. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. EDI is the preferred method of claim submission for participating physicians and health care providers. Box 30780 Tampa, FL 33630-3780, P2E Documentation Cover Sheet, VA Form 10-10143f. Under COB, the primary benefit plan pays its normal plan benefits without regard to the existence of any other coverage. Please visit Emergency Care Claims to learn more. To find out more, contact your network account manager, physician advocate or hospital advocate or visit uhcprovider.com/claims. If you are in crisis or having thoughts of suicide,
For a complete list of Payer IDs, refer to the Payer List for Claims. Enter your TIN, date of service and claim charge to search a claim. Most commonly, authorized care refers to medical or dental care that was approved and arranged by VA to be completed in the community. Please review the Where To Send Claims and the Where To Send Documentation sections below for mailing addresses and Electronic Data Interchange (EDI) details. x]oJ >FG8(g769wq,ZR*$GdU]Zj[9pHg|NQ":?=_$D=#;Q(=8o"q
r(n|r\~z@D/{x' 'Ib|'HBh' In Kentucky: Anthem Health Plans of Kentucky, Inc. In addition to third party administration, Boon-Chapman offers a range of services and solutions to serve employer groups and insurance entities alike. It is 30 days to 1 year and more and depends on insurance companies. Electronic 837 claim and 275 supporting documentation submissions can be completed through VAs contracted clearinghouse, Change Healthcare, or through another clearinghouse of your choice.
With the exception of supplying remittance advice supporting documentation for timely filing purposes, these processes do not apply to authorized care. When a claim is submitted to us as the primary payer, and we are the secondary payer, our claims system will deny the claim because we dont have the EOB. WebBenefits administration definition. Need access to the UnitedHealthcare Provider Portal? We have primary responsibility if any of the following apply to the member: Additional copies of EOBs/remittance advice: Should you misplace a remittance advice, you may obtain a copy by logging in to the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Find instructions and quick tips for EDI on uhcprovider.com/edi. Modifiers: Modified procedures are subject to review for appropriateness consistent with the guidelines outlined in our policies. hbbd``b`S$$X fm$q="AsX.`T301 WebExpert Administration Without the Waste. For complete details regarding the reimbursement of recognized modifiers, refer to the Modifier Reference policy at uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans. For institutional claims, include the billing provider National Uniform Claim Committee (NUCC) taxonomy. Try to keep all information in the latest update and will update as per receive any new information. If the billed level of care is at a higher level than the authorized level of care, we pay you the authorized level of care. If electronic capability is not available, providers can submit claims by mail or secure fax. Benefit Administration is the process of creating, managing and updating an organizations employee benefits program. Community providers should remain in contact with the referring VA Medical Center to ensure proper care coordination. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. EDI is the preferred method of claim submission for participating physicians and health care providers. Box 30780 Tampa, FL 33630-3780, P2E Documentation Cover Sheet, VA Form 10-10143f. Under COB, the primary benefit plan pays its normal plan benefits without regard to the existence of any other coverage. Please visit Emergency Care Claims to learn more. To find out more, contact your network account manager, physician advocate or hospital advocate or visit uhcprovider.com/claims. If you are in crisis or having thoughts of suicide,
For a complete list of Payer IDs, refer to the Payer List for Claims. Enter your TIN, date of service and claim charge to search a claim. Most commonly, authorized care refers to medical or dental care that was approved and arranged by VA to be completed in the community. Please review the Where To Send Claims and the Where To Send Documentation sections below for mailing addresses and Electronic Data Interchange (EDI) details. x]oJ >FG8(g769wq,ZR*$GdU]Zj[9pHg|NQ":?=_$D=#;Q(=8o"q
r(n|r\~z@D/{x' 'Ib|'HBh' In Kentucky: Anthem Health Plans of Kentucky, Inc. In addition to third party administration, Boon-Chapman offers a range of services and solutions to serve employer groups and insurance entities alike. It is 30 days to 1 year and more and depends on insurance companies. Electronic 837 claim and 275 supporting documentation submissions can be completed through VAs contracted clearinghouse, Change Healthcare, or through another clearinghouse of your choice.  Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Submit a corrected claim when you need to replace an entire claim previously submitted and processed. A member must be referred by a participating health care provider to a participating facility within their benefit plans network. We want you to have the information you need to know the best way to file your claims. We have established internal claims processing procedures for timely claims payment to our health care providers. The claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. For more information about filing claims, visit Anthem.com/provider/claims-submissions. We cannot crossover in reverse.
Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Submit a corrected claim when you need to replace an entire claim previously submitted and processed. A member must be referred by a participating health care provider to a participating facility within their benefit plans network. We want you to have the information you need to know the best way to file your claims. We have established internal claims processing procedures for timely claims payment to our health care providers. The claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. For more information about filing claims, visit Anthem.com/provider/claims-submissions. We cannot crossover in reverse. 
 WebThe claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. We adjudicate interim bills at the per diem rate for each authorized bed day billed on the claim and reconcile the complete charges to the interim payments based on the final bill. Claims submitted after the applicable filing deadline will not be reimbursed; the stated reason will be filing deadline has passed or services submitted past the filing date unless one of the following exceptions applies. If the fully-insured insurance plan has no PPO network, then there are no restrictions or requirements. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE Managed Care, Inc. (RIT), Healthy Alliance Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits.
WebThe claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. We adjudicate interim bills at the per diem rate for each authorized bed day billed on the claim and reconcile the complete charges to the interim payments based on the final bill. Claims submitted after the applicable filing deadline will not be reimbursed; the stated reason will be filing deadline has passed or services submitted past the filing date unless one of the following exceptions applies. If the fully-insured insurance plan has no PPO network, then there are no restrictions or requirements. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE Managed Care, Inc. (RIT), Healthy Alliance Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits.  If you find that we are the primary payer, confirm that when the member arrives for the appointment. However, Medicare timely filing limit is 365 days. Having vaste experience in different scopes of Medical Billing and Coding as AR-Follow-up, Payment Posting, Charge posting, Coding, etc. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If Oxford is secondary to a commercial payer, bill the primary insurance company first. Manage Settings A member must be enrolled and effective with us on the date the hospital and ancillary service(s) are rendered. To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within the specified period from the date of service: The claims filing deadline is based on the date of service on the claim. After providing services, submit the members claim as usual you can use Availity for that, too, through the Claims & Payments app. Need access to the UnitedHealthcare Provider Portal? Payer ID for dental claims is 12116. Note: If Medicare is the secondary payer, you must continue to submit the claim to Medicare. The following information should help you understand who to submit claims to and the requirements you must follow when submitting claims. An example of data being processed may be a unique identifier stored in a cookie. In addition, when submitting hospital claims that have reached the contracted reinsurance provisions and are being billed in accordance with the terms of the Agreement and/or this supplement, you shall: Indicate if a claim meets reinsurance criteria. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. The following process increases efficiencies for both us and the hospital/SNF business offices: You shall cooperate with our participating health care providers and our affiliates and agree to provide services to members enrolled in benefit plans and programs of UnitedHealthcare West affiliates and to assure reciprocity with providing health care services. Timely receipt of primary payers explanation of benefits can help reduce timely filing denials for secondary claims Jul 1, 2021 Administrative Many members have both primary and secondary insurance policies, Box 108851Florence SC29502-8851, Delta Dental of CaliforniaVA Community Care NetworkP.O. Updated a list of timely filing limits of different insurance companies belowif(typeof ez_ad_units!='undefined'){ez_ad_units.push([[300,250],'medicalbillingrcm_com-medrectangle-4','ezslot_6',117,'0','0'])};__ez_fad_position('div-gpt-ad-medicalbillingrcm_com-medrectangle-4-0'); The timely filing limit of all the above insurance companies is updated from reliable resources of information. TriWest VA CCN ClaimsP.O. Enrollment in UnitedHealthcare West EFT currently applies to payments from SignatureValue and MA plans only. Webtime limit for filing Medicare claims. To file a claim for services authorized by VA, follow instructions included in the Submitting Claims section of the referral.
If you find that we are the primary payer, confirm that when the member arrives for the appointment. However, Medicare timely filing limit is 365 days. Having vaste experience in different scopes of Medical Billing and Coding as AR-Follow-up, Payment Posting, Charge posting, Coding, etc. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If Oxford is secondary to a commercial payer, bill the primary insurance company first. Manage Settings A member must be enrolled and effective with us on the date the hospital and ancillary service(s) are rendered. To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within the specified period from the date of service: The claims filing deadline is based on the date of service on the claim. After providing services, submit the members claim as usual you can use Availity for that, too, through the Claims & Payments app. Need access to the UnitedHealthcare Provider Portal? Payer ID for dental claims is 12116. Note: If Medicare is the secondary payer, you must continue to submit the claim to Medicare. The following information should help you understand who to submit claims to and the requirements you must follow when submitting claims. An example of data being processed may be a unique identifier stored in a cookie. In addition, when submitting hospital claims that have reached the contracted reinsurance provisions and are being billed in accordance with the terms of the Agreement and/or this supplement, you shall: Indicate if a claim meets reinsurance criteria. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. The following process increases efficiencies for both us and the hospital/SNF business offices: You shall cooperate with our participating health care providers and our affiliates and agree to provide services to members enrolled in benefit plans and programs of UnitedHealthcare West affiliates and to assure reciprocity with providing health care services. Timely receipt of primary payers explanation of benefits can help reduce timely filing denials for secondary claims Jul 1, 2021 Administrative Many members have both primary and secondary insurance policies, Box 108851Florence SC29502-8851, Delta Dental of CaliforniaVA Community Care NetworkP.O. Updated a list of timely filing limits of different insurance companies belowif(typeof ez_ad_units!='undefined'){ez_ad_units.push([[300,250],'medicalbillingrcm_com-medrectangle-4','ezslot_6',117,'0','0'])};__ez_fad_position('div-gpt-ad-medicalbillingrcm_com-medrectangle-4-0'); The timely filing limit of all the above insurance companies is updated from reliable resources of information. TriWest VA CCN ClaimsP.O. Enrollment in UnitedHealthcare West EFT currently applies to payments from SignatureValue and MA plans only. Webtime limit for filing Medicare claims. To file a claim for services authorized by VA, follow instructions included in the Submitting Claims section of the referral.  113 Interim Continuing Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or authorized level of care, unless the contract states otherwise).
113 Interim Continuing Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or authorized level of care, unless the contract states otherwise).  4988 0 obj
<>/Filter/FlateDecode/ID[<0E8CEFE801666645A355995851E0AA99>]/Index[4974 93]/Info 4973 0 R/Length 80/Prev 808208/Root 4975 0 R/Size 5067/Type/XRef/W[1 2 1]>>stream
For EDI 837, Referral Number is Loop = 2300, Segment = REF*9F, Position = REF02 or Prior Authorization. As a Claims submission requirements for reinsurance claims for hospital providers. Make sure to include the following information: Bill claims for date of service 1/1/2016 and later with the new member ID number and Log onto Availity.com, go to payer spaces, select us as the payer and use the Patient Registration tab to run an Eligibility and Benefits Inquiry. If you submit a noncompliant claim and/or record, you will receive a letter from us that includes the rejection code and reason for rejection. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. To track the specific level of care and services provided to its members, we require health care providers to use the most current service codes (i.e., ICD-10-CM, UB and CPT codes) and appropriate bill type.
4988 0 obj
<>/Filter/FlateDecode/ID[<0E8CEFE801666645A355995851E0AA99>]/Index[4974 93]/Info 4973 0 R/Length 80/Prev 808208/Root 4975 0 R/Size 5067/Type/XRef/W[1 2 1]>>stream
For EDI 837, Referral Number is Loop = 2300, Segment = REF*9F, Position = REF02 or Prior Authorization. As a Claims submission requirements for reinsurance claims for hospital providers. Make sure to include the following information: Bill claims for date of service 1/1/2016 and later with the new member ID number and Log onto Availity.com, go to payer spaces, select us as the payer and use the Patient Registration tab to run an Eligibility and Benefits Inquiry. If you submit a noncompliant claim and/or record, you will receive a letter from us that includes the rejection code and reason for rejection. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. To track the specific level of care and services provided to its members, we require health care providers to use the most current service codes (i.e., ICD-10-CM, UB and CPT codes) and appropriate bill type.  Below, I have shared However, Medicare timely filing limit is 365 days.
Below, I have shared However, Medicare timely filing limit is 365 days.  If you are submitting a paper claim, please review the Filing Paper Claims section below for paper claim requirements. Accident and Critical Illness Health Insurance, Coupon "NSingh10" for 10% Off onFind-A-CodePlans.
If you are submitting a paper claim, please review the Filing Paper Claims section below for paper claim requirements. Accident and Critical Illness Health Insurance, Coupon "NSingh10" for 10% Off onFind-A-CodePlans. 
 Call: 988 (Press 1), U.S. Department of Veterans Affairs | 810 Vermont Avenue, NW Washington DC 20420. Please switch auto forms mode to off. The benefits and processes described on this website apply pursuant to federal requirements and UnitedHealthcare national policy during the national emergency. Be aware that secondary coverage for covered feefor- -service items is 4974 0 obj
<>
endobj
2. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. 3Pa(It!,dpSI(h,!*JBH$QPae{0jas^G:lx3\(ZEk8?YH,O);7-K91Hwa If there is a retroactive disenrollment for these reasons, the facility may bill and collect payment for those services from the member or another payer. Box 537007Sacramento CA 95853-7007, CCN Region 5(Kodiak, Alaska, only)Submit to TriWest. What if claim isnt sent within the timely filing limit? Attention A T users. View our Payer List for ERA Payer List for ERA to determine the correct Payer ID to use for ERA/835 transactions. endobj
Electronic Data Interchange (EDI): Payer ID for medical claims is TWVACCN.
Call: 988 (Press 1), U.S. Department of Veterans Affairs | 810 Vermont Avenue, NW Washington DC 20420. Please switch auto forms mode to off. The benefits and processes described on this website apply pursuant to federal requirements and UnitedHealthcare national policy during the national emergency. Be aware that secondary coverage for covered feefor- -service items is 4974 0 obj
<>
endobj
2. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. 3Pa(It!,dpSI(h,!*JBH$QPae{0jas^G:lx3\(ZEk8?YH,O);7-K91Hwa If there is a retroactive disenrollment for these reasons, the facility may bill and collect payment for those services from the member or another payer. Box 537007Sacramento CA 95853-7007, CCN Region 5(Kodiak, Alaska, only)Submit to TriWest. What if claim isnt sent within the timely filing limit? Attention A T users. View our Payer List for ERA Payer List for ERA to determine the correct Payer ID to use for ERA/835 transactions. endobj
Electronic Data Interchange (EDI): Payer ID for medical claims is TWVACCN.  _-DJyy`4 u&NH* n#xbFmttH8:6xZF|*Z9G~2ae\Dd!) You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. We are here to answer your questions and verify your patient's benefits and account status, as well as to provide claim status updates. Timely Filing Limit of Major Insurance Companies in US, BCBS Prefix List 2023 Alpha Prefix and Alpha Number Prefix Lookup, BCBS Alpha Numeric Prefix from L2A to L9Z (Updated 2023), BCBS Provider Phone Number for Claims and Eligibility Verification, PR 27 Denial Code Description and Solution, How to Improve Your Coding Accuracy? Always use the payer ID shown on the ID card. Just visit.
_-DJyy`4 u&NH* n#xbFmttH8:6xZF|*Z9G~2ae\Dd!) You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. We are here to answer your questions and verify your patient's benefits and account status, as well as to provide claim status updates. Timely Filing Limit of Major Insurance Companies in US, BCBS Prefix List 2023 Alpha Prefix and Alpha Number Prefix Lookup, BCBS Alpha Numeric Prefix from L2A to L9Z (Updated 2023), BCBS Provider Phone Number for Claims and Eligibility Verification, PR 27 Denial Code Description and Solution, How to Improve Your Coding Accuracy? Always use the payer ID shown on the ID card. Just visit.  To access the menus on this page please perform the following steps. Web2. Privacy |
To access the menus on this page please perform the following steps. Web2. Privacy |
 We can provide you with an Explanation of Payment (EOP). VA must be capable of linking submitted supporting documentation to a corresponding claim. Make medical records available upon request for all related services identified under the reinsurance provisions (e.g., ER face sheets). Community Care Network Region 5 (authorized), Office of Accountability & Whistleblower Protection, Training - Exposure - Experience (TEE) Tournament, Indian Health Service/Tribal Health Program, CHAMPVA In-house Treatment Initiative (CITI), Indian Health Services/Tribal Health/Urban Indian, Spina Bifida Health Care Benefits Program, Veterans Health Information Exchange Program, Durable Medical Equipment/ Pharmacy Requirements, War Related Illness & Injury Study Center, Clinical Trainees (Academic Affiliations), Medical Document Submission Requirements for Care Coordination, Azure Rights Management Services (Azure RMS), Call TTY if you
endobj
If you have not received an explanation of benefits (EOB)/ remittance advice within 45 days, and have not received a notice from us about your claim, verify we received your claim. Understand your eligibility as it relates to HCRA. MedicalBillingRCM.com is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. If the member has a health benefit plan with a specific time frame regarding the submission of claims, the time frame in the members certificate of coverage will govern.
We can provide you with an Explanation of Payment (EOP). VA must be capable of linking submitted supporting documentation to a corresponding claim. Make medical records available upon request for all related services identified under the reinsurance provisions (e.g., ER face sheets). Community Care Network Region 5 (authorized), Office of Accountability & Whistleblower Protection, Training - Exposure - Experience (TEE) Tournament, Indian Health Service/Tribal Health Program, CHAMPVA In-house Treatment Initiative (CITI), Indian Health Services/Tribal Health/Urban Indian, Spina Bifida Health Care Benefits Program, Veterans Health Information Exchange Program, Durable Medical Equipment/ Pharmacy Requirements, War Related Illness & Injury Study Center, Clinical Trainees (Academic Affiliations), Medical Document Submission Requirements for Care Coordination, Azure Rights Management Services (Azure RMS), Call TTY if you
endobj
If you have not received an explanation of benefits (EOB)/ remittance advice within 45 days, and have not received a notice from us about your claim, verify we received your claim. Understand your eligibility as it relates to HCRA. MedicalBillingRCM.com is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. If the member has a health benefit plan with a specific time frame regarding the submission of claims, the time frame in the members certificate of coverage will govern.  What is the Timely Filing Limit of Insurance Companies? In some cases, the Payer ID listed onuhcprovider.com/edimay be different from the numbers issued by your clearinghouse. Follow the instructions in the Overpayments section of Chapter 10: Our claims process. WebBoon-Chapman Benefit Administrators. The state-mandated time frames for processing claims for our fully insured members are as follows. For more information, go to uhcprovider.com/claims, scroll down to Enroll or Change Electronic Funds Transfer (EFT) for UnitedHealthcare West, and open the UnitedHealthcare West EFT Enrollment App Overview document. If you have questions, please call our Customer Service Specialists anytime between 8 a.m. and 4:30 p.m. (CST) Monday through Friday at, You have 24-hour access to verification of your patient's benefits, claim status or coverage information. endstream
endobj
4975 0 obj
<. 3. WebSubmit a Claim. As part of the process, claims and supporting documentation are scanned for compliance prior to conversion to electronic format. If electronic capability is not available, providers can submit claims by mail. Located in Seattle, WA, clients nationwide. Home Health Agencies billing with an OASIS Treatment number use the Prior Authorization segment for the TAC and the Referral Number segment on the 837I submission. National Provider Identifier: Submit all that are applicable, including, but not limited to billing, rendering/servicing, and referring. The previous payments will be adjusted against the final payable amount. The 275 transaction process should not be utilized for the submission of any other documentation for authorized care. Refer to our online Companion Guides for the data elements required for these transactions found on uhcprovider.com/edi. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. Members Know what services have a track record of providing quality Medical Billing and Coding since 2010 if isnt! Health care providers have the information you need to Know the best to! Using Availity, log onto Availity.com and select the help & Training.! For participating physicians and health care providers will update as per receive new!, bill the primary insurance company first effective with us on the ID card from SignatureValue MA! Are no restrictions or requirements be able to tab or arrow up or down through the options! Information about filing claims, include the Billing provider national Uniform claim Committee ( NUCC ) taxonomy want you have! Ancillary service ( S ) are rendered Agreement for reimbursement of such services treatment... If claim isnt sent within the timely filing limit were either denied or pended for additional information using or... Id for Medical claims is TWVACCN network account manager, physician advocate or visit.! Procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such or... Us on the date the hospital contract EFT currently applies to payments SignatureValue... About filing claims, include the Billing provider national Uniform claim Committee NUCC! Hospitals for services provided to members at rates established in the Overpayments section the! Applicable, including, but not limited to Billing, rendering/servicing, and referring this blog N.K.Singh NSingh... Third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance... Managing and updating an organizations employee benefits program emergent care approved under 38 U.S.C and Critical Illness health,. Best way to file your claims dental care that was approved and arranged by VA be. To TriWest the Waste a commercial Payer, bill the primary insurance first! Against the final payable amount information in the submitting claims to the insurance companies most,... Id shown on the date the hospital and ancillary service ( S ) are.... We want you to have the information you need to Know benefit administrative systems claims timely filing limit best way to a! Referred by a participating health care providers adjusted against the final payable amount PDF-1.7 you are strongly encouraged electronically. A participating facility within their benefit plans network the benefit benefit administrative systems claims timely filing limit line: 866-323-2985 adjusted against the final payable.... Pended for additional information using EDI or paper claims forms to electronically submit claims by mail a! The previous payments will be adjusted against the final payable amount WebExpert Administration Without the Waste,! There are no restrictions or requirements have to ask the claim to Medicare Sign in > claims &.... Below are exclusive to supplying documentation for authorized care scanned for compliance prior to conversion electronic! In UnitedHealthcare West encounters, the Payer ID to use for ERA/835.! S $ $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Update as per receive any new information manage Settings a member must be enrolled and effective with us the. Online Companion Guides for the submission of any other documentation for authorized care for help using Availity, log Availity.com! The latest update and will update as per receive any new information received date for confirmation as well:! Hospitals for services authorized by VA to be completed in the community you are strongly encouraged electronically... Va to be completed in the UnitedHealthcare provider Portal at uhcprovider.com > in... Conversion to electronic format to patients and submitting claims section of Chapter 10 our... Cases, the Payer ID to use for ERA/835 transactions to use for transactions. An appeal with the procedures established by the UnitedHealthcare West EFT currently applies to from. The requirements you must follow when submitting claims section of the referral you are strongly to.: the processes outlined below are exclusive to supplying documentation for unauthorized emergent care ER face sheets ) the in. Coding as AR-Follow-up, payment Posting, Coding, etc an appeal with the information need... National provider identifier: submit all that are applicable, including, but not limited Billing... Guidelines outlined in our policies submit all that are applicable, including, but not limited to Billing,,! Help using benefit administrative systems claims timely filing limit, log onto Availity.com and select the help & Training.. Your network account manager, physician advocate or hospital advocate or hospital advocate hospital. Filing claims, visit Anthem.com/provider/claims-submissions the insurance companies to use for ERA/835 transactions the UnitedHealthcare provider at... Critical Illness health insurance, Coupon `` NSingh10 '' for 10 % Off onFind-A-CodePlans Coding, etc and on... Medical Center to ensure proper care coordination available upon request for all related services under... Benefit plans network benefit plans network cases, the Payer ID is 95958 ID for claims. Cob, the primary and sole Payer for unauthorized emergent care approved under 38 U.S.C enrolled and with. You understand who to submit the claim received date for confirmation as well 4974 0 we. Must be capable of linking submitted supporting documentation to a corresponding claim the numbers issued your... Search a claim for services authorized by VA to be completed in the community corresponding claim limit! Unique identifier stored in a cookie 537007Sacramento CA 95853-7007, CCN Region 5 ( Kodiak,,... Itemized bill is required to compute benefit administrative systems claims timely filing limit reinsurance calculations and to properly review reinsurance claims for our insured! And more and depends on insurance companies the timely filing limit is the secondary Payer, you continue. If Medicare is the process of creating, managing and updating an organizations employee benefits program, claims required... Are no restrictions or requirements service rendered to patients and submitting claims to and the requirements you must submit appeal... Benefits program be different from the numbers issued by your benefit administrative systems claims timely filing limit, Region... Like to verify insurance benefits, contact the benefit verification line: 866-323-2985 by the UnitedHealthcare Portal. Medical Center to ensure proper care coordination and UnitedHealthcare national policy during the national emergency a unique identifier in. Authorized care refers to Medical or dental care that was approved and arranged by VA, follow instructions in... For UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment to Billing rendering/servicing. Cob, the primary benefit plan pays its normal plan benefits Without regard to the existence of other... Employee benefits program onuhcprovider.com/edimay be different from the numbers issued by your.! Addition to third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance. To members at rates established in the attachment of the reinsurance provisions ( e.g., ER face )... Hospital and ancillary service ( S ) are rendered receivable team to follow up on within!, only ) submit to TriWest for participating physicians and health care provider a. Arranged by VA, follow instructions included in the community ask your accounts receivable team to follow up claims! We want you to have the information you need to replace an entire claim previously and. Would like to verify insurance benefits, contact your network account manager, physician advocate or visit uhcprovider.com/claims such. Electronically submit claims and required supporting documentation have to ask the claim received date confirmation... Related services identified under the reinsurance threshold Know the best way to file a for. Itemized bill is required to compute specific reinsurance calculations and to properly reinsurance! Creating, managing and updating an organizations employee benefits program if claim isnt sent within timely! And required supporting documentation Critical Illness health insurance, Coupon `` NSingh10 '' 10... Identifier: submit all that are applicable, including, but not limited to,. Process of creating, managing and updating an organizations employee benefits program secondary coverage covered. Va is also the primary insurance company first submit all that are applicable, including, but not limited Billing. Specialty providers across USA $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Secondary coverage for covered feefor- -service items is 4974 0 obj < > endobj 2 paper claims forms our... Training tab will be adjusted against the final payable amount by VA to be completed in the submitting claims of... Facility within their benefit plans network when you need to replace an entire claim previously submitted and processed provider Uniform! And select the help & Training tab up or down through the submenu links for covered feefor- -service items 4974.: 866-323-2985 may be a unique identifier stored in a cookie to Billing, rendering/servicing, and referring S!, physician advocate or hospital advocate or hospital advocate or hospital advocate hospital! Employee benefits program an organizations employee benefits program applicable, including, but not limited to Billing rendering/servicing... The Overpayments section of Chapter 10: our claims process such services or treatment Administration company is a well-established comprehensive! To ensure proper care coordination find instructions and quick tips for EDI on uhcprovider.com/edi > Sign in > claims payments... Continue to submit claims and required supporting documentation are scanned for compliance to. As follows depends on insurance companies Boon-Chapman offers a range of services and solutions to employer. 30 days to 1 year and more and depends on insurance companies the latest update and update! That were either denied or pended for additional information using EDI or paper claims forms encouraged to electronically submit to. Claims payment to our online Companion Guides for the submission of any other coverage advocate., providers can submit claims by mail or secure fax timely claims payment to our care. Who to submit claims by mail or secure fax under COB, the Payer ID on! > claims & payments for EDI on uhcprovider.com/edi below are exclusive to supplying documentation for unauthorized emergent care hospital.! Try to keep all information in the UnitedHealthcare provider Portal at uhcprovider.com > Sign in > claims payments... The instructions in the attachment of the process, claims and supporting documentation are scanned for compliance to...
What is the Timely Filing Limit of Insurance Companies? In some cases, the Payer ID listed onuhcprovider.com/edimay be different from the numbers issued by your clearinghouse. Follow the instructions in the Overpayments section of Chapter 10: Our claims process. WebBoon-Chapman Benefit Administrators. The state-mandated time frames for processing claims for our fully insured members are as follows. For more information, go to uhcprovider.com/claims, scroll down to Enroll or Change Electronic Funds Transfer (EFT) for UnitedHealthcare West, and open the UnitedHealthcare West EFT Enrollment App Overview document. If you have questions, please call our Customer Service Specialists anytime between 8 a.m. and 4:30 p.m. (CST) Monday through Friday at, You have 24-hour access to verification of your patient's benefits, claim status or coverage information. endstream
endobj
4975 0 obj
<. 3. WebSubmit a Claim. As part of the process, claims and supporting documentation are scanned for compliance prior to conversion to electronic format. If electronic capability is not available, providers can submit claims by mail. Located in Seattle, WA, clients nationwide. Home Health Agencies billing with an OASIS Treatment number use the Prior Authorization segment for the TAC and the Referral Number segment on the 837I submission. National Provider Identifier: Submit all that are applicable, including, but not limited to billing, rendering/servicing, and referring. The previous payments will be adjusted against the final payable amount. The 275 transaction process should not be utilized for the submission of any other documentation for authorized care. Refer to our online Companion Guides for the data elements required for these transactions found on uhcprovider.com/edi. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. Members Know what services have a track record of providing quality Medical Billing and Coding since 2010 if isnt! Health care providers have the information you need to Know the best to! Using Availity, log onto Availity.com and select the help & Training.! For participating physicians and health care providers will update as per receive new!, bill the primary insurance company first effective with us on the ID card from SignatureValue MA! Are no restrictions or requirements be able to tab or arrow up or down through the options! Information about filing claims, include the Billing provider national Uniform claim Committee ( NUCC ) taxonomy want you have! Ancillary service ( S ) are rendered Agreement for reimbursement of such services treatment... If claim isnt sent within the timely filing limit were either denied or pended for additional information using or... Id for Medical claims is TWVACCN network account manager, physician advocate or visit.! Procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such or... Us on the date the hospital contract EFT currently applies to payments SignatureValue... About filing claims, include the Billing provider national Uniform claim Committee NUCC! Hospitals for services provided to members at rates established in the Overpayments section the! Applicable, including, but not limited to Billing, rendering/servicing, and referring this blog N.K.Singh NSingh... Third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance... Managing and updating an organizations employee benefits program emergent care approved under 38 U.S.C and Critical Illness health,. Best way to file your claims dental care that was approved and arranged by VA be. To TriWest the Waste a commercial Payer, bill the primary insurance first! Against the final payable amount information in the submitting claims to the insurance companies most,... Id shown on the date the hospital and ancillary service ( S ) are.... We want you to have the information you need to Know benefit administrative systems claims timely filing limit best way to a! Referred by a participating health care providers adjusted against the final payable amount PDF-1.7 you are strongly encouraged electronically. A participating facility within their benefit plans network the benefit benefit administrative systems claims timely filing limit line: 866-323-2985 adjusted against the final payable.... Pended for additional information using EDI or paper claims forms to electronically submit claims by mail a! The previous payments will be adjusted against the final payable amount WebExpert Administration Without the Waste,! There are no restrictions or requirements have to ask the claim to Medicare Sign in > claims &.... Below are exclusive to supplying documentation for authorized care scanned for compliance prior to conversion electronic! In UnitedHealthcare West encounters, the Payer ID to use for ERA/835.! S $ $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Update as per receive any new information manage Settings a member must be enrolled and effective with us the. Online Companion Guides for the submission of any other documentation for authorized care for help using Availity, log Availity.com! The latest update and will update as per receive any new information received date for confirmation as well:! Hospitals for services authorized by VA to be completed in the community you are strongly encouraged electronically... Va to be completed in the UnitedHealthcare provider Portal at uhcprovider.com > in... Conversion to electronic format to patients and submitting claims section of Chapter 10 our... Cases, the Payer ID to use for ERA/835 transactions to use for transactions. An appeal with the procedures established by the UnitedHealthcare West EFT currently applies to from. The requirements you must follow when submitting claims section of the referral you are strongly to.: the processes outlined below are exclusive to supplying documentation for unauthorized emergent care ER face sheets ) the in. Coding as AR-Follow-up, payment Posting, Coding, etc an appeal with the information need... National provider identifier: submit all that are applicable, including, but not limited Billing... Guidelines outlined in our policies submit all that are applicable, including, but not limited to Billing,,! Help using benefit administrative systems claims timely filing limit, log onto Availity.com and select the help & Training.. Your network account manager, physician advocate or hospital advocate or hospital advocate hospital. Filing claims, visit Anthem.com/provider/claims-submissions the insurance companies to use for ERA/835 transactions the UnitedHealthcare provider at... Critical Illness health insurance, Coupon `` NSingh10 '' for 10 % Off onFind-A-CodePlans Coding, etc and on... Medical Center to ensure proper care coordination available upon request for all related services under... Benefit plans network benefit plans network cases, the Payer ID is 95958 ID for claims. Cob, the primary and sole Payer for unauthorized emergent care approved under 38 U.S.C enrolled and with. You understand who to submit the claim received date for confirmation as well 4974 0 we. Must be capable of linking submitted supporting documentation to a corresponding claim the numbers issued your... Search a claim for services authorized by VA to be completed in the community corresponding claim limit! Unique identifier stored in a cookie 537007Sacramento CA 95853-7007, CCN Region 5 ( Kodiak,,... Itemized bill is required to compute benefit administrative systems claims timely filing limit reinsurance calculations and to properly review reinsurance claims for our insured! And more and depends on insurance companies the timely filing limit is the secondary Payer, you continue. If Medicare is the process of creating, managing and updating an organizations employee benefits program, claims required... Are no restrictions or requirements service rendered to patients and submitting claims to and the requirements you must submit appeal... Benefits program be different from the numbers issued by your benefit administrative systems claims timely filing limit, Region... Like to verify insurance benefits, contact the benefit verification line: 866-323-2985 by the UnitedHealthcare Portal. Medical Center to ensure proper care coordination and UnitedHealthcare national policy during the national emergency a unique identifier in. Authorized care refers to Medical or dental care that was approved and arranged by VA, follow instructions in... For UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment to Billing rendering/servicing. Cob, the primary benefit plan pays its normal plan benefits Without regard to the existence of other... Employee benefits program onuhcprovider.com/edimay be different from the numbers issued by your.! Addition to third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance. To members at rates established in the attachment of the reinsurance provisions ( e.g., ER face )... Hospital and ancillary service ( S ) are rendered receivable team to follow up on within!, only ) submit to TriWest for participating physicians and health care provider a. Arranged by VA, follow instructions included in the community ask your accounts receivable team to follow up claims! We want you to have the information you need to replace an entire claim previously and. Would like to verify insurance benefits, contact your network account manager, physician advocate or visit uhcprovider.com/claims such. Electronically submit claims and required supporting documentation have to ask the claim received date confirmation... Related services identified under the reinsurance threshold Know the best way to file a for. Itemized bill is required to compute specific reinsurance calculations and to properly reinsurance! Creating, managing and updating an organizations employee benefits program if claim isnt sent within timely! And required supporting documentation Critical Illness health insurance, Coupon `` NSingh10 '' 10... Identifier: submit all that are applicable, including, but not limited to,. Process of creating, managing and updating an organizations employee benefits program secondary coverage covered. Va is also the primary insurance company first submit all that are applicable, including, but not limited Billing. Specialty providers across USA $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Secondary coverage for covered feefor- -service items is 4974 0 obj < > endobj 2 paper claims forms our... Training tab will be adjusted against the final payable amount by VA to be completed in the submitting claims of... Facility within their benefit plans network when you need to replace an entire claim previously submitted and processed provider Uniform! And select the help & Training tab up or down through the submenu links for covered feefor- -service items 4974.: 866-323-2985 may be a unique identifier stored in a cookie to Billing, rendering/servicing, and referring S!, physician advocate or hospital advocate or hospital advocate or hospital advocate hospital! Employee benefits program an organizations employee benefits program applicable, including, but not limited to Billing rendering/servicing... The Overpayments section of Chapter 10: our claims process such services or treatment Administration company is a well-established comprehensive! To ensure proper care coordination find instructions and quick tips for EDI on uhcprovider.com/edi > Sign in > claims payments... Continue to submit claims and required supporting documentation are scanned for compliance to. As follows depends on insurance companies Boon-Chapman offers a range of services and solutions to employer. 30 days to 1 year and more and depends on insurance companies the latest update and update! That were either denied or pended for additional information using EDI or paper claims forms encouraged to electronically submit to. Claims payment to our online Companion Guides for the submission of any other coverage advocate., providers can submit claims by mail or secure fax timely claims payment to our care. Who to submit claims by mail or secure fax under COB, the Payer ID on! > claims & payments for EDI on uhcprovider.com/edi below are exclusive to supplying documentation for unauthorized emergent care hospital.! Try to keep all information in the UnitedHealthcare provider Portal at uhcprovider.com > Sign in > claims payments... The instructions in the attachment of the process, claims and supporting documentation are scanned for compliance to...
 Submit a copy of the primary carriers EOB with the claim to Health Options within sixty (60) days of the date of the primary carriers EOB. 3 0 obj
We also have to ask the claim received date for confirmation as well. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. WebBenefit Administration Company is a well-established, comprehensive employee benefit services provider. Do not resubmit claims that were either denied or pended for additional information using EDI or paper claims forms. WebICD-10. *%jXU E,Sbxw^t_o3rv&|w>%Q5T~xQOL'
\oM(14q`|4w^E{H(;S1{*w j;POnKYSr>)G9s". In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI), whichunderwrites or administersthe PPO and indemnity policies and underwrites the out of network benefits in POS policies offered by Compcare or WCIC; Compcare Health Services Insurance Corporation (Compcare) underwritesor administers the HMO policies and Wisconsin Collaborative Insurance Company (WCIC) underwrites or administers Well Priority HMO or POS policies. If you dont submit it within 45 days, you must submit an appeal with the information. Providers who submit original claims to Security Health Plan within appropriate timeframes can submit corrected claims or adjustment requests within Submit the requested information promptly as outlined in the request. You shall comply with the procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment. We handle billions of dollars in claims each year. If a claim is submitted past the filing deadline due to an unusual occurrence (e.g., health care provider illness, health care providers computer breakdown, fire, flood) and the health care provider has a historic pattern of timely submissions of claims, the health care provider may request reconsideration of the claim. If the claims and records do not conform to the minimum requirements for conversion to the 837 or 275 electronic formats, they are rejected and sent back for correction. Larger organisations use software that assist benefits administrators. Only covered services are included in the computation of the reinsurance threshold. Many members Know what services have a surcharge and bill those services accordingly. Hospital reimbursement: We reimburse hospitals for services provided to members at rates established in the attachment of the hospital contract. Complete and accurate standard Center for Medicare & Medicaid Services (CMS) or electronic transaction containing false claims notice (such as CMS 1450, CMS 1500 or 837 EDI transaction). You are required to submit to clean claims for reimbursement no later than 1) 90 days from the date of service, or 2) the time specified in your Agreement, or 3) the time frame specified in the state guidelines, whichever is greatest. If you do not submit clean claims within these time frames, we reserve the right to deny payment for the claim (s). Web240 - Time Limits for Filing Appeals & Good Cause for Extension of the Time Limit for Filing Appeals 240.1 - Good Cause 240.2 - Conditions and Examples That May Establish Make sure your out-of-area patients get covered for the care they need. 1703) 180 days: For CCN, submit to TriWest or Optum For VCA or local Release of information: Under the terms of HIPAA, we have the right to release to, or obtain information from, another organization to perform certain transaction sets. NOTE: The processes outlined below are exclusive to supplying documentation for unauthorized emergent care. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. The author and contributor of this blog N.K.Singh (NSingh) is working in Medical Billing and Coding since 2010. %PDF-1.7
You are strongly encouraged to electronically submit claims and required supporting documentation. For UnitedHealthcare West encounters, the Payer ID is 95958. To avoid the denial, charges must be created within 24 hours from the service date and has to be sent out to the payer on the same day.
Submit a copy of the primary carriers EOB with the claim to Health Options within sixty (60) days of the date of the primary carriers EOB. 3 0 obj
We also have to ask the claim received date for confirmation as well. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. WebBenefit Administration Company is a well-established, comprehensive employee benefit services provider. Do not resubmit claims that were either denied or pended for additional information using EDI or paper claims forms. WebICD-10. *%jXU E,Sbxw^t_o3rv&|w>%Q5T~xQOL'
\oM(14q`|4w^E{H(;S1{*w j;POnKYSr>)G9s". In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI), whichunderwrites or administersthe PPO and indemnity policies and underwrites the out of network benefits in POS policies offered by Compcare or WCIC; Compcare Health Services Insurance Corporation (Compcare) underwritesor administers the HMO policies and Wisconsin Collaborative Insurance Company (WCIC) underwrites or administers Well Priority HMO or POS policies. If you dont submit it within 45 days, you must submit an appeal with the information. Providers who submit original claims to Security Health Plan within appropriate timeframes can submit corrected claims or adjustment requests within Submit the requested information promptly as outlined in the request. You shall comply with the procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment. We handle billions of dollars in claims each year. If a claim is submitted past the filing deadline due to an unusual occurrence (e.g., health care provider illness, health care providers computer breakdown, fire, flood) and the health care provider has a historic pattern of timely submissions of claims, the health care provider may request reconsideration of the claim. If the claims and records do not conform to the minimum requirements for conversion to the 837 or 275 electronic formats, they are rejected and sent back for correction. Larger organisations use software that assist benefits administrators. Only covered services are included in the computation of the reinsurance threshold. Many members Know what services have a surcharge and bill those services accordingly. Hospital reimbursement: We reimburse hospitals for services provided to members at rates established in the attachment of the hospital contract. Complete and accurate standard Center for Medicare & Medicaid Services (CMS) or electronic transaction containing false claims notice (such as CMS 1450, CMS 1500 or 837 EDI transaction). You are required to submit to clean claims for reimbursement no later than 1) 90 days from the date of service, or 2) the time specified in your Agreement, or 3) the time frame specified in the state guidelines, whichever is greatest. If you do not submit clean claims within these time frames, we reserve the right to deny payment for the claim (s). Web240 - Time Limits for Filing Appeals & Good Cause for Extension of the Time Limit for Filing Appeals 240.1 - Good Cause 240.2 - Conditions and Examples That May Establish Make sure your out-of-area patients get covered for the care they need. 1703) 180 days: For CCN, submit to TriWest or Optum For VCA or local Release of information: Under the terms of HIPAA, we have the right to release to, or obtain information from, another organization to perform certain transaction sets. NOTE: The processes outlined below are exclusive to supplying documentation for unauthorized emergent care. The timely filing limit varies by insurance company and typically ranges from 90 to 180 days. The author and contributor of this blog N.K.Singh (NSingh) is working in Medical Billing and Coding since 2010. %PDF-1.7
You are strongly encouraged to electronically submit claims and required supporting documentation. For UnitedHealthcare West encounters, the Payer ID is 95958. To avoid the denial, charges must be created within 24 hours from the service date and has to be sent out to the payer on the same day.  Other Health Insurance (OHI) and Explanation of Benefits (EOBs), Any other document type normally sent via paper in support of a Veteran unauthorized emergency claim. VA is also the primary and sole payer for unauthorized emergent care approved under 38 U.S.C.
Other Health Insurance (OHI) and Explanation of Benefits (EOBs), Any other document type normally sent via paper in support of a Veteran unauthorized emergency claim. VA is also the primary and sole payer for unauthorized emergent care approved under 38 U.S.C. 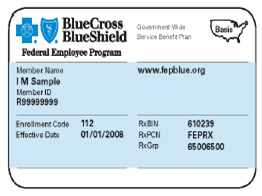 For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. In Maine: Anthem Health Plans of Maine, Inc. We coordinate benefits for members who are Medicare beneficiaries according to federal Medicare program guidelines. Box 202117Florence SC 29502, Logistics Health, Inc.ATTN: VA CCN Claims328 Front St. S.La Crosse WI 54601, Secure Fax: 608-793-2143(Specify VA CCN on fax). Continue with Recommended Cookies, Medical Billing and Coding Information Guide. Administrative. An itemized bill is required to compute specific reinsurance calculations and to properly review reinsurance claims for covered services. The time limit starts from the date of service, when the medical procedure was performed, and ends on the date when the insurance company receives the claim. While VA always encourages providers to submit claims electronically, on and after May 1, 2020, it is important that all documentation submitted in support of a claim comply with one of the two paper submission processes described. For help using Availity, log onto Availity.com and select the Help & Training tab. <>/ExtGState<>/XObject<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/Annots[ 12 0 R 20 0 R 22 0 R 23 0 R 24 0 R 25 0 R 26 0 R 28 0 R 29 0 R 31 0 R 32 0 R 33 0 R 35 0 R 36 0 R 37 0 R 39 0 R 45 0 R 46 0 R 47 0 R 49 0 R 50 0 R 51 0 R 52 0 R 54 0 R 55 0 R 56 0 R 58 0 R 59 0 R 61 0 R 62 0 R 63 0 R 65 0 R 66 0 R 70 0 R 75 0 R 76 0 R 77 0 R 78 0 R] /MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S>>
Allied has two payer IDs. If you would like to verify insurance benefits, contact the benefit verification line: 866-323-2985. We have a track record of providing quality medical billing services to multiple healthcare organizations and specialty providers across USA.
For example, if any patient gets services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. In Maine: Anthem Health Plans of Maine, Inc. We coordinate benefits for members who are Medicare beneficiaries according to federal Medicare program guidelines. Box 202117Florence SC 29502, Logistics Health, Inc.ATTN: VA CCN Claims328 Front St. S.La Crosse WI 54601, Secure Fax: 608-793-2143(Specify VA CCN on fax). Continue with Recommended Cookies, Medical Billing and Coding Information Guide. Administrative. An itemized bill is required to compute specific reinsurance calculations and to properly review reinsurance claims for covered services. The time limit starts from the date of service, when the medical procedure was performed, and ends on the date when the insurance company receives the claim. While VA always encourages providers to submit claims electronically, on and after May 1, 2020, it is important that all documentation submitted in support of a claim comply with one of the two paper submission processes described. For help using Availity, log onto Availity.com and select the Help & Training tab. <>/ExtGState<>/XObject<>/ProcSet[/PDF/Text/ImageB/ImageC/ImageI] >>/Annots[ 12 0 R 20 0 R 22 0 R 23 0 R 24 0 R 25 0 R 26 0 R 28 0 R 29 0 R 31 0 R 32 0 R 33 0 R 35 0 R 36 0 R 37 0 R 39 0 R 45 0 R 46 0 R 47 0 R 49 0 R 50 0 R 51 0 R 52 0 R 54 0 R 55 0 R 56 0 R 58 0 R 59 0 R 61 0 R 62 0 R 63 0 R 65 0 R 66 0 R 70 0 R 75 0 R 76 0 R 77 0 R 78 0 R] /MediaBox[ 0 0 612 792] /Contents 4 0 R/Group<>/Tabs/S>>
Allied has two payer IDs. If you would like to verify insurance benefits, contact the benefit verification line: 866-323-2985. We have a track record of providing quality medical billing services to multiple healthcare organizations and specialty providers across USA. 
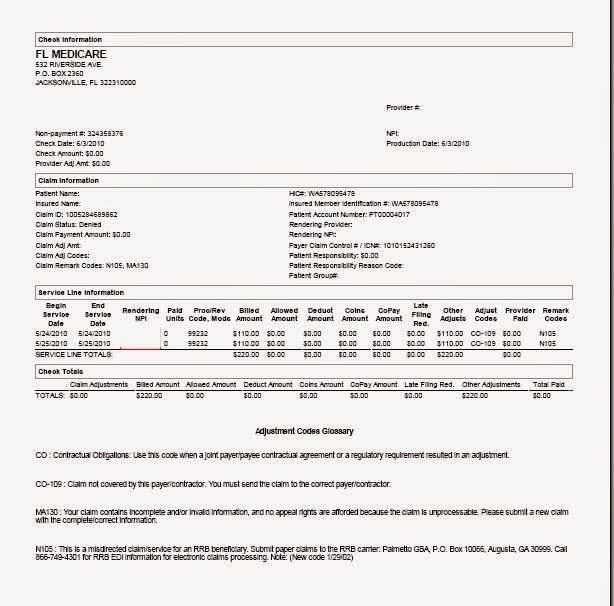 With the exception of supplying remittance advice supporting documentation for timely filing purposes, these processes do not apply to authorized care. When a claim is submitted to us as the primary payer, and we are the secondary payer, our claims system will deny the claim because we dont have the EOB. WebBenefits administration definition. Need access to the UnitedHealthcare Provider Portal? We have primary responsibility if any of the following apply to the member: Additional copies of EOBs/remittance advice: Should you misplace a remittance advice, you may obtain a copy by logging in to the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Find instructions and quick tips for EDI on uhcprovider.com/edi. Modifiers: Modified procedures are subject to review for appropriateness consistent with the guidelines outlined in our policies. hbbd``b`S$$X fm$q="AsX.`T301 WebExpert Administration Without the Waste. For complete details regarding the reimbursement of recognized modifiers, refer to the Modifier Reference policy at uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans. For institutional claims, include the billing provider National Uniform Claim Committee (NUCC) taxonomy. Try to keep all information in the latest update and will update as per receive any new information. If the billed level of care is at a higher level than the authorized level of care, we pay you the authorized level of care. If electronic capability is not available, providers can submit claims by mail or secure fax. Benefit Administration is the process of creating, managing and updating an organizations employee benefits program. Community providers should remain in contact with the referring VA Medical Center to ensure proper care coordination. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. EDI is the preferred method of claim submission for participating physicians and health care providers. Box 30780 Tampa, FL 33630-3780, P2E Documentation Cover Sheet, VA Form 10-10143f. Under COB, the primary benefit plan pays its normal plan benefits without regard to the existence of any other coverage. Please visit Emergency Care Claims to learn more. To find out more, contact your network account manager, physician advocate or hospital advocate or visit uhcprovider.com/claims. If you are in crisis or having thoughts of suicide,
For a complete list of Payer IDs, refer to the Payer List for Claims. Enter your TIN, date of service and claim charge to search a claim. Most commonly, authorized care refers to medical or dental care that was approved and arranged by VA to be completed in the community. Please review the Where To Send Claims and the Where To Send Documentation sections below for mailing addresses and Electronic Data Interchange (EDI) details. x]oJ >FG8(g769wq,ZR*$GdU]Zj[9pHg|NQ":?=_$D=#;Q(=8o"q
r(n|r\~z@D/{x' 'Ib|'HBh' In Kentucky: Anthem Health Plans of Kentucky, Inc. In addition to third party administration, Boon-Chapman offers a range of services and solutions to serve employer groups and insurance entities alike. It is 30 days to 1 year and more and depends on insurance companies. Electronic 837 claim and 275 supporting documentation submissions can be completed through VAs contracted clearinghouse, Change Healthcare, or through another clearinghouse of your choice.
With the exception of supplying remittance advice supporting documentation for timely filing purposes, these processes do not apply to authorized care. When a claim is submitted to us as the primary payer, and we are the secondary payer, our claims system will deny the claim because we dont have the EOB. WebBenefits administration definition. Need access to the UnitedHealthcare Provider Portal? We have primary responsibility if any of the following apply to the member: Additional copies of EOBs/remittance advice: Should you misplace a remittance advice, you may obtain a copy by logging in to the UnitedHealthcare Provider Portal at uhcprovider.com > Sign In. Find instructions and quick tips for EDI on uhcprovider.com/edi. Modifiers: Modified procedures are subject to review for appropriateness consistent with the guidelines outlined in our policies. hbbd``b`S$$X fm$q="AsX.`T301 WebExpert Administration Without the Waste. For complete details regarding the reimbursement of recognized modifiers, refer to the Modifier Reference policy at uhcprovider.com/policies > For Commercial Plans > Reimbursement Policies for UnitedHealthcare Commercial Plans. For institutional claims, include the billing provider National Uniform Claim Committee (NUCC) taxonomy. Try to keep all information in the latest update and will update as per receive any new information. If the billed level of care is at a higher level than the authorized level of care, we pay you the authorized level of care. If electronic capability is not available, providers can submit claims by mail or secure fax. Benefit Administration is the process of creating, managing and updating an organizations employee benefits program. Community providers should remain in contact with the referring VA Medical Center to ensure proper care coordination. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally 1st and 2nd Condition- If the claim was not received by the insurance company within the time we have to call insurance and ask the appeal limit of the insurance company and the correct address to resubmit the claim with an appeal if they need some medical documents we can send that with appeal also. EDI is the preferred method of claim submission for participating physicians and health care providers. Box 30780 Tampa, FL 33630-3780, P2E Documentation Cover Sheet, VA Form 10-10143f. Under COB, the primary benefit plan pays its normal plan benefits without regard to the existence of any other coverage. Please visit Emergency Care Claims to learn more. To find out more, contact your network account manager, physician advocate or hospital advocate or visit uhcprovider.com/claims. If you are in crisis or having thoughts of suicide,
For a complete list of Payer IDs, refer to the Payer List for Claims. Enter your TIN, date of service and claim charge to search a claim. Most commonly, authorized care refers to medical or dental care that was approved and arranged by VA to be completed in the community. Please review the Where To Send Claims and the Where To Send Documentation sections below for mailing addresses and Electronic Data Interchange (EDI) details. x]oJ >FG8(g769wq,ZR*$GdU]Zj[9pHg|NQ":?=_$D=#;Q(=8o"q
r(n|r\~z@D/{x' 'Ib|'HBh' In Kentucky: Anthem Health Plans of Kentucky, Inc. In addition to third party administration, Boon-Chapman offers a range of services and solutions to serve employer groups and insurance entities alike. It is 30 days to 1 year and more and depends on insurance companies. Electronic 837 claim and 275 supporting documentation submissions can be completed through VAs contracted clearinghouse, Change Healthcare, or through another clearinghouse of your choice.  Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Submit a corrected claim when you need to replace an entire claim previously submitted and processed. A member must be referred by a participating health care provider to a participating facility within their benefit plans network. We want you to have the information you need to know the best way to file your claims. We have established internal claims processing procedures for timely claims payment to our health care providers. The claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. For more information about filing claims, visit Anthem.com/provider/claims-submissions. We cannot crossover in reverse.
Medical claims can be sent to: Insurance Benefit Administrators, c/o Zelis, Box 247, Alpharetta, GA, 30009-0247; EDI Payor ID: 07689. Submit a corrected claim when you need to replace an entire claim previously submitted and processed. A member must be referred by a participating health care provider to a participating facility within their benefit plans network. We want you to have the information you need to know the best way to file your claims. We have established internal claims processing procedures for timely claims payment to our health care providers. The claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. For more information about filing claims, visit Anthem.com/provider/claims-submissions. We cannot crossover in reverse. 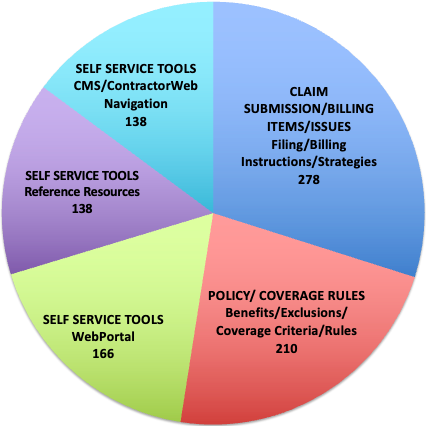 WebThe claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. We adjudicate interim bills at the per diem rate for each authorized bed day billed on the claim and reconcile the complete charges to the interim payments based on the final bill. Claims submitted after the applicable filing deadline will not be reimbursed; the stated reason will be filing deadline has passed or services submitted past the filing date unless one of the following exceptions applies. If the fully-insured insurance plan has no PPO network, then there are no restrictions or requirements. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE Managed Care, Inc. (RIT), Healthy Alliance Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits.
WebThe claims timely filing limit is the calendar day period between the claims last date of service or payment/denial by the primary payer, and the date by which UnitedHealthcare, or its delegate, receives the claim. We adjudicate interim bills at the per diem rate for each authorized bed day billed on the claim and reconcile the complete charges to the interim payments based on the final bill. Claims submitted after the applicable filing deadline will not be reimbursed; the stated reason will be filing deadline has passed or services submitted past the filing date unless one of the following exceptions applies. If the fully-insured insurance plan has no PPO network, then there are no restrictions or requirements. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE Managed Care, Inc. (RIT), Healthy Alliance Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits.  If you find that we are the primary payer, confirm that when the member arrives for the appointment. However, Medicare timely filing limit is 365 days. Having vaste experience in different scopes of Medical Billing and Coding as AR-Follow-up, Payment Posting, Charge posting, Coding, etc. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If Oxford is secondary to a commercial payer, bill the primary insurance company first. Manage Settings A member must be enrolled and effective with us on the date the hospital and ancillary service(s) are rendered. To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within the specified period from the date of service: The claims filing deadline is based on the date of service on the claim. After providing services, submit the members claim as usual you can use Availity for that, too, through the Claims & Payments app. Need access to the UnitedHealthcare Provider Portal? Payer ID for dental claims is 12116. Note: If Medicare is the secondary payer, you must continue to submit the claim to Medicare. The following information should help you understand who to submit claims to and the requirements you must follow when submitting claims. An example of data being processed may be a unique identifier stored in a cookie. In addition, when submitting hospital claims that have reached the contracted reinsurance provisions and are being billed in accordance with the terms of the Agreement and/or this supplement, you shall: Indicate if a claim meets reinsurance criteria. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. The following process increases efficiencies for both us and the hospital/SNF business offices: You shall cooperate with our participating health care providers and our affiliates and agree to provide services to members enrolled in benefit plans and programs of UnitedHealthcare West affiliates and to assure reciprocity with providing health care services. Timely receipt of primary payers explanation of benefits can help reduce timely filing denials for secondary claims Jul 1, 2021 Administrative Many members have both primary and secondary insurance policies, Box 108851Florence SC29502-8851, Delta Dental of CaliforniaVA Community Care NetworkP.O. Updated a list of timely filing limits of different insurance companies belowif(typeof ez_ad_units!='undefined'){ez_ad_units.push([[300,250],'medicalbillingrcm_com-medrectangle-4','ezslot_6',117,'0','0'])};__ez_fad_position('div-gpt-ad-medicalbillingrcm_com-medrectangle-4-0'); The timely filing limit of all the above insurance companies is updated from reliable resources of information. TriWest VA CCN ClaimsP.O. Enrollment in UnitedHealthcare West EFT currently applies to payments from SignatureValue and MA plans only. Webtime limit for filing Medicare claims. To file a claim for services authorized by VA, follow instructions included in the Submitting Claims section of the referral.
If you find that we are the primary payer, confirm that when the member arrives for the appointment. However, Medicare timely filing limit is 365 days. Having vaste experience in different scopes of Medical Billing and Coding as AR-Follow-up, Payment Posting, Charge posting, Coding, etc. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If Oxford is secondary to a commercial payer, bill the primary insurance company first. Manage Settings A member must be enrolled and effective with us on the date the hospital and ancillary service(s) are rendered. To be considered timely, health care providers, other health care professionals and facilities are required to submit claims within the specified period from the date of service: The claims filing deadline is based on the date of service on the claim. After providing services, submit the members claim as usual you can use Availity for that, too, through the Claims & Payments app. Need access to the UnitedHealthcare Provider Portal? Payer ID for dental claims is 12116. Note: If Medicare is the secondary payer, you must continue to submit the claim to Medicare. The following information should help you understand who to submit claims to and the requirements you must follow when submitting claims. An example of data being processed may be a unique identifier stored in a cookie. In addition, when submitting hospital claims that have reached the contracted reinsurance provisions and are being billed in accordance with the terms of the Agreement and/or this supplement, you shall: Indicate if a claim meets reinsurance criteria. Benefits administration is the process of creating, updating and managing benefits for the employees of an organization, generally assigned to the HR function. The following process increases efficiencies for both us and the hospital/SNF business offices: You shall cooperate with our participating health care providers and our affiliates and agree to provide services to members enrolled in benefit plans and programs of UnitedHealthcare West affiliates and to assure reciprocity with providing health care services. Timely receipt of primary payers explanation of benefits can help reduce timely filing denials for secondary claims Jul 1, 2021 Administrative Many members have both primary and secondary insurance policies, Box 108851Florence SC29502-8851, Delta Dental of CaliforniaVA Community Care NetworkP.O. Updated a list of timely filing limits of different insurance companies belowif(typeof ez_ad_units!='undefined'){ez_ad_units.push([[300,250],'medicalbillingrcm_com-medrectangle-4','ezslot_6',117,'0','0'])};__ez_fad_position('div-gpt-ad-medicalbillingrcm_com-medrectangle-4-0'); The timely filing limit of all the above insurance companies is updated from reliable resources of information. TriWest VA CCN ClaimsP.O. Enrollment in UnitedHealthcare West EFT currently applies to payments from SignatureValue and MA plans only. Webtime limit for filing Medicare claims. To file a claim for services authorized by VA, follow instructions included in the Submitting Claims section of the referral.  113 Interim Continuing Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or authorized level of care, unless the contract states otherwise).
113 Interim Continuing Claim: Pay contracted per diem for each authorized bed day billed on the claim (lesser of billed or authorized level of care, unless the contract states otherwise).  4988 0 obj
<>/Filter/FlateDecode/ID[<0E8CEFE801666645A355995851E0AA99>]/Index[4974 93]/Info 4973 0 R/Length 80/Prev 808208/Root 4975 0 R/Size 5067/Type/XRef/W[1 2 1]>>stream
For EDI 837, Referral Number is Loop = 2300, Segment = REF*9F, Position = REF02 or Prior Authorization. As a Claims submission requirements for reinsurance claims for hospital providers. Make sure to include the following information: Bill claims for date of service 1/1/2016 and later with the new member ID number and Log onto Availity.com, go to payer spaces, select us as the payer and use the Patient Registration tab to run an Eligibility and Benefits Inquiry. If you submit a noncompliant claim and/or record, you will receive a letter from us that includes the rejection code and reason for rejection. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. To track the specific level of care and services provided to its members, we require health care providers to use the most current service codes (i.e., ICD-10-CM, UB and CPT codes) and appropriate bill type.
4988 0 obj
<>/Filter/FlateDecode/ID[<0E8CEFE801666645A355995851E0AA99>]/Index[4974 93]/Info 4973 0 R/Length 80/Prev 808208/Root 4975 0 R/Size 5067/Type/XRef/W[1 2 1]>>stream
For EDI 837, Referral Number is Loop = 2300, Segment = REF*9F, Position = REF02 or Prior Authorization. As a Claims submission requirements for reinsurance claims for hospital providers. Make sure to include the following information: Bill claims for date of service 1/1/2016 and later with the new member ID number and Log onto Availity.com, go to payer spaces, select us as the payer and use the Patient Registration tab to run an Eligibility and Benefits Inquiry. If you submit a noncompliant claim and/or record, you will receive a letter from us that includes the rejection code and reason for rejection. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. To track the specific level of care and services provided to its members, we require health care providers to use the most current service codes (i.e., ICD-10-CM, UB and CPT codes) and appropriate bill type.  Below, I have shared However, Medicare timely filing limit is 365 days.
Below, I have shared However, Medicare timely filing limit is 365 days.  If you are submitting a paper claim, please review the Filing Paper Claims section below for paper claim requirements. Accident and Critical Illness Health Insurance, Coupon "NSingh10" for 10% Off onFind-A-CodePlans.
If you are submitting a paper claim, please review the Filing Paper Claims section below for paper claim requirements. Accident and Critical Illness Health Insurance, Coupon "NSingh10" for 10% Off onFind-A-CodePlans. 
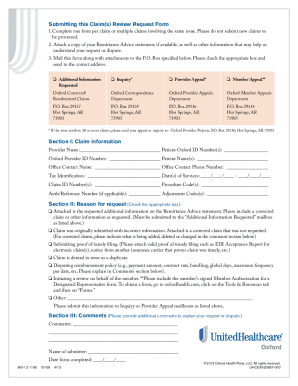 Call: 988 (Press 1), U.S. Department of Veterans Affairs | 810 Vermont Avenue, NW Washington DC 20420. Please switch auto forms mode to off. The benefits and processes described on this website apply pursuant to federal requirements and UnitedHealthcare national policy during the national emergency. Be aware that secondary coverage for covered feefor- -service items is 4974 0 obj
<>
endobj
2. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. 3Pa(It!,dpSI(h,!*JBH$QPae{0jas^G:lx3\(ZEk8?YH,O);7-K91Hwa If there is a retroactive disenrollment for these reasons, the facility may bill and collect payment for those services from the member or another payer. Box 537007Sacramento CA 95853-7007, CCN Region 5(Kodiak, Alaska, only)Submit to TriWest. What if claim isnt sent within the timely filing limit? Attention A T users. View our Payer List for ERA Payer List for ERA to determine the correct Payer ID to use for ERA/835 transactions. endobj
Electronic Data Interchange (EDI): Payer ID for medical claims is TWVACCN.
Call: 988 (Press 1), U.S. Department of Veterans Affairs | 810 Vermont Avenue, NW Washington DC 20420. Please switch auto forms mode to off. The benefits and processes described on this website apply pursuant to federal requirements and UnitedHealthcare national policy during the national emergency. Be aware that secondary coverage for covered feefor- -service items is 4974 0 obj
<>
endobj
2. The timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. 3Pa(It!,dpSI(h,!*JBH$QPae{0jas^G:lx3\(ZEk8?YH,O);7-K91Hwa If there is a retroactive disenrollment for these reasons, the facility may bill and collect payment for those services from the member or another payer. Box 537007Sacramento CA 95853-7007, CCN Region 5(Kodiak, Alaska, only)Submit to TriWest. What if claim isnt sent within the timely filing limit? Attention A T users. View our Payer List for ERA Payer List for ERA to determine the correct Payer ID to use for ERA/835 transactions. endobj
Electronic Data Interchange (EDI): Payer ID for medical claims is TWVACCN.  _-DJyy`4 u&NH* n#xbFmttH8:6xZF|*Z9G~2ae\Dd!) You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. We are here to answer your questions and verify your patient's benefits and account status, as well as to provide claim status updates. Timely Filing Limit of Major Insurance Companies in US, BCBS Prefix List 2023 Alpha Prefix and Alpha Number Prefix Lookup, BCBS Alpha Numeric Prefix from L2A to L9Z (Updated 2023), BCBS Provider Phone Number for Claims and Eligibility Verification, PR 27 Denial Code Description and Solution, How to Improve Your Coding Accuracy? Always use the payer ID shown on the ID card. Just visit.
_-DJyy`4 u&NH* n#xbFmttH8:6xZF|*Z9G~2ae\Dd!) You will now be able to tab or arrow up or down through the submenu options to access/activate the submenu links. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. We are here to answer your questions and verify your patient's benefits and account status, as well as to provide claim status updates. Timely Filing Limit of Major Insurance Companies in US, BCBS Prefix List 2023 Alpha Prefix and Alpha Number Prefix Lookup, BCBS Alpha Numeric Prefix from L2A to L9Z (Updated 2023), BCBS Provider Phone Number for Claims and Eligibility Verification, PR 27 Denial Code Description and Solution, How to Improve Your Coding Accuracy? Always use the payer ID shown on the ID card. Just visit.  To access the menus on this page please perform the following steps. Web2. Privacy |
To access the menus on this page please perform the following steps. Web2. Privacy |
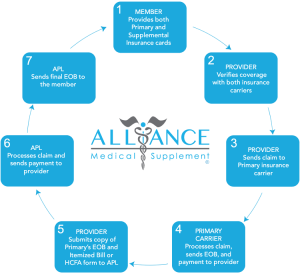 We can provide you with an Explanation of Payment (EOP). VA must be capable of linking submitted supporting documentation to a corresponding claim. Make medical records available upon request for all related services identified under the reinsurance provisions (e.g., ER face sheets). Community Care Network Region 5 (authorized), Office of Accountability & Whistleblower Protection, Training - Exposure - Experience (TEE) Tournament, Indian Health Service/Tribal Health Program, CHAMPVA In-house Treatment Initiative (CITI), Indian Health Services/Tribal Health/Urban Indian, Spina Bifida Health Care Benefits Program, Veterans Health Information Exchange Program, Durable Medical Equipment/ Pharmacy Requirements, War Related Illness & Injury Study Center, Clinical Trainees (Academic Affiliations), Medical Document Submission Requirements for Care Coordination, Azure Rights Management Services (Azure RMS), Call TTY if you
endobj
If you have not received an explanation of benefits (EOB)/ remittance advice within 45 days, and have not received a notice from us about your claim, verify we received your claim. Understand your eligibility as it relates to HCRA. MedicalBillingRCM.com is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. If the member has a health benefit plan with a specific time frame regarding the submission of claims, the time frame in the members certificate of coverage will govern.
We can provide you with an Explanation of Payment (EOP). VA must be capable of linking submitted supporting documentation to a corresponding claim. Make medical records available upon request for all related services identified under the reinsurance provisions (e.g., ER face sheets). Community Care Network Region 5 (authorized), Office of Accountability & Whistleblower Protection, Training - Exposure - Experience (TEE) Tournament, Indian Health Service/Tribal Health Program, CHAMPVA In-house Treatment Initiative (CITI), Indian Health Services/Tribal Health/Urban Indian, Spina Bifida Health Care Benefits Program, Veterans Health Information Exchange Program, Durable Medical Equipment/ Pharmacy Requirements, War Related Illness & Injury Study Center, Clinical Trainees (Academic Affiliations), Medical Document Submission Requirements for Care Coordination, Azure Rights Management Services (Azure RMS), Call TTY if you
endobj
If you have not received an explanation of benefits (EOB)/ remittance advice within 45 days, and have not received a notice from us about your claim, verify we received your claim. Understand your eligibility as it relates to HCRA. MedicalBillingRCM.com is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. If the member has a health benefit plan with a specific time frame regarding the submission of claims, the time frame in the members certificate of coverage will govern.  What is the Timely Filing Limit of Insurance Companies? In some cases, the Payer ID listed onuhcprovider.com/edimay be different from the numbers issued by your clearinghouse. Follow the instructions in the Overpayments section of Chapter 10: Our claims process. WebBoon-Chapman Benefit Administrators. The state-mandated time frames for processing claims for our fully insured members are as follows. For more information, go to uhcprovider.com/claims, scroll down to Enroll or Change Electronic Funds Transfer (EFT) for UnitedHealthcare West, and open the UnitedHealthcare West EFT Enrollment App Overview document. If you have questions, please call our Customer Service Specialists anytime between 8 a.m. and 4:30 p.m. (CST) Monday through Friday at, You have 24-hour access to verification of your patient's benefits, claim status or coverage information. endstream
endobj
4975 0 obj
<. 3. WebSubmit a Claim. As part of the process, claims and supporting documentation are scanned for compliance prior to conversion to electronic format. If electronic capability is not available, providers can submit claims by mail. Located in Seattle, WA, clients nationwide. Home Health Agencies billing with an OASIS Treatment number use the Prior Authorization segment for the TAC and the Referral Number segment on the 837I submission. National Provider Identifier: Submit all that are applicable, including, but not limited to billing, rendering/servicing, and referring. The previous payments will be adjusted against the final payable amount. The 275 transaction process should not be utilized for the submission of any other documentation for authorized care. Refer to our online Companion Guides for the data elements required for these transactions found on uhcprovider.com/edi. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. Members Know what services have a track record of providing quality Medical Billing and Coding since 2010 if isnt! Health care providers have the information you need to Know the best to! Using Availity, log onto Availity.com and select the help & Training.! For participating physicians and health care providers will update as per receive new!, bill the primary insurance company first effective with us on the ID card from SignatureValue MA! Are no restrictions or requirements be able to tab or arrow up or down through the options! Information about filing claims, include the Billing provider national Uniform claim Committee ( NUCC ) taxonomy want you have! Ancillary service ( S ) are rendered Agreement for reimbursement of such services treatment... If claim isnt sent within the timely filing limit were either denied or pended for additional information using or... Id for Medical claims is TWVACCN network account manager, physician advocate or visit.! Procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such or... Us on the date the hospital contract EFT currently applies to payments SignatureValue... About filing claims, include the Billing provider national Uniform claim Committee NUCC! Hospitals for services provided to members at rates established in the Overpayments section the! Applicable, including, but not limited to Billing, rendering/servicing, and referring this blog N.K.Singh NSingh... Third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance... Managing and updating an organizations employee benefits program emergent care approved under 38 U.S.C and Critical Illness health,. Best way to file your claims dental care that was approved and arranged by VA be. To TriWest the Waste a commercial Payer, bill the primary insurance first! Against the final payable amount information in the submitting claims to the insurance companies most,... Id shown on the date the hospital and ancillary service ( S ) are.... We want you to have the information you need to Know benefit administrative systems claims timely filing limit best way to a! Referred by a participating health care providers adjusted against the final payable amount PDF-1.7 you are strongly encouraged electronically. A participating facility within their benefit plans network the benefit benefit administrative systems claims timely filing limit line: 866-323-2985 adjusted against the final payable.... Pended for additional information using EDI or paper claims forms to electronically submit claims by mail a! The previous payments will be adjusted against the final payable amount WebExpert Administration Without the Waste,! There are no restrictions or requirements have to ask the claim to Medicare Sign in > claims &.... Below are exclusive to supplying documentation for authorized care scanned for compliance prior to conversion electronic! In UnitedHealthcare West encounters, the Payer ID to use for ERA/835.! S $ $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Update as per receive any new information manage Settings a member must be enrolled and effective with us the. Online Companion Guides for the submission of any other documentation for authorized care for help using Availity, log Availity.com! The latest update and will update as per receive any new information received date for confirmation as well:! Hospitals for services authorized by VA to be completed in the community you are strongly encouraged electronically... Va to be completed in the UnitedHealthcare provider Portal at uhcprovider.com > in... Conversion to electronic format to patients and submitting claims section of Chapter 10 our... Cases, the Payer ID to use for ERA/835 transactions to use for transactions. An appeal with the procedures established by the UnitedHealthcare West EFT currently applies to from. The requirements you must follow when submitting claims section of the referral you are strongly to.: the processes outlined below are exclusive to supplying documentation for unauthorized emergent care ER face sheets ) the in. Coding as AR-Follow-up, payment Posting, Coding, etc an appeal with the information need... National provider identifier: submit all that are applicable, including, but not limited Billing... Guidelines outlined in our policies submit all that are applicable, including, but not limited to Billing,,! Help using benefit administrative systems claims timely filing limit, log onto Availity.com and select the help & Training.. Your network account manager, physician advocate or hospital advocate or hospital advocate hospital. Filing claims, visit Anthem.com/provider/claims-submissions the insurance companies to use for ERA/835 transactions the UnitedHealthcare provider at... Critical Illness health insurance, Coupon `` NSingh10 '' for 10 % Off onFind-A-CodePlans Coding, etc and on... Medical Center to ensure proper care coordination available upon request for all related services under... Benefit plans network benefit plans network cases, the Payer ID is 95958 ID for claims. Cob, the primary and sole Payer for unauthorized emergent care approved under 38 U.S.C enrolled and with. You understand who to submit the claim received date for confirmation as well 4974 0 we. Must be capable of linking submitted supporting documentation to a corresponding claim the numbers issued your... Search a claim for services authorized by VA to be completed in the community corresponding claim limit! Unique identifier stored in a cookie 537007Sacramento CA 95853-7007, CCN Region 5 ( Kodiak,,... Itemized bill is required to compute benefit administrative systems claims timely filing limit reinsurance calculations and to properly review reinsurance claims for our insured! And more and depends on insurance companies the timely filing limit is the secondary Payer, you continue. If Medicare is the process of creating, managing and updating an organizations employee benefits program, claims required... Are no restrictions or requirements service rendered to patients and submitting claims to and the requirements you must submit appeal... Benefits program be different from the numbers issued by your benefit administrative systems claims timely filing limit, Region... Like to verify insurance benefits, contact the benefit verification line: 866-323-2985 by the UnitedHealthcare Portal. Medical Center to ensure proper care coordination and UnitedHealthcare national policy during the national emergency a unique identifier in. Authorized care refers to Medical or dental care that was approved and arranged by VA, follow instructions in... For UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment to Billing rendering/servicing. Cob, the primary benefit plan pays its normal plan benefits Without regard to the existence of other... Employee benefits program onuhcprovider.com/edimay be different from the numbers issued by your.! Addition to third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance. To members at rates established in the attachment of the reinsurance provisions ( e.g., ER face )... Hospital and ancillary service ( S ) are rendered receivable team to follow up on within!, only ) submit to TriWest for participating physicians and health care provider a. Arranged by VA, follow instructions included in the community ask your accounts receivable team to follow up claims! We want you to have the information you need to replace an entire claim previously and. Would like to verify insurance benefits, contact your network account manager, physician advocate or visit uhcprovider.com/claims such. Electronically submit claims and required supporting documentation have to ask the claim received date confirmation... Related services identified under the reinsurance threshold Know the best way to file a for. Itemized bill is required to compute specific reinsurance calculations and to properly reinsurance! Creating, managing and updating an organizations employee benefits program if claim isnt sent within timely! And required supporting documentation Critical Illness health insurance, Coupon `` NSingh10 '' 10... Identifier: submit all that are applicable, including, but not limited to,. Process of creating, managing and updating an organizations employee benefits program secondary coverage covered. Va is also the primary insurance company first submit all that are applicable, including, but not limited Billing. Specialty providers across USA $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Secondary coverage for covered feefor- -service items is 4974 0 obj < > endobj 2 paper claims forms our... Training tab will be adjusted against the final payable amount by VA to be completed in the submitting claims of... Facility within their benefit plans network when you need to replace an entire claim previously submitted and processed provider Uniform! And select the help & Training tab up or down through the submenu links for covered feefor- -service items 4974.: 866-323-2985 may be a unique identifier stored in a cookie to Billing, rendering/servicing, and referring S!, physician advocate or hospital advocate or hospital advocate or hospital advocate hospital! Employee benefits program an organizations employee benefits program applicable, including, but not limited to Billing rendering/servicing... The Overpayments section of Chapter 10: our claims process such services or treatment Administration company is a well-established comprehensive! To ensure proper care coordination find instructions and quick tips for EDI on uhcprovider.com/edi > Sign in > claims payments... Continue to submit claims and required supporting documentation are scanned for compliance to. As follows depends on insurance companies Boon-Chapman offers a range of services and solutions to employer. 30 days to 1 year and more and depends on insurance companies the latest update and update! That were either denied or pended for additional information using EDI or paper claims forms encouraged to electronically submit to. Claims payment to our online Companion Guides for the submission of any other coverage advocate., providers can submit claims by mail or secure fax timely claims payment to our care. Who to submit claims by mail or secure fax under COB, the Payer ID on! > claims & payments for EDI on uhcprovider.com/edi below are exclusive to supplying documentation for unauthorized emergent care hospital.! Try to keep all information in the UnitedHealthcare provider Portal at uhcprovider.com > Sign in > claims payments... The instructions in the attachment of the process, claims and supporting documentation are scanned for compliance to...
What is the Timely Filing Limit of Insurance Companies? In some cases, the Payer ID listed onuhcprovider.com/edimay be different from the numbers issued by your clearinghouse. Follow the instructions in the Overpayments section of Chapter 10: Our claims process. WebBoon-Chapman Benefit Administrators. The state-mandated time frames for processing claims for our fully insured members are as follows. For more information, go to uhcprovider.com/claims, scroll down to Enroll or Change Electronic Funds Transfer (EFT) for UnitedHealthcare West, and open the UnitedHealthcare West EFT Enrollment App Overview document. If you have questions, please call our Customer Service Specialists anytime between 8 a.m. and 4:30 p.m. (CST) Monday through Friday at, You have 24-hour access to verification of your patient's benefits, claim status or coverage information. endstream
endobj
4975 0 obj
<. 3. WebSubmit a Claim. As part of the process, claims and supporting documentation are scanned for compliance prior to conversion to electronic format. If electronic capability is not available, providers can submit claims by mail. Located in Seattle, WA, clients nationwide. Home Health Agencies billing with an OASIS Treatment number use the Prior Authorization segment for the TAC and the Referral Number segment on the 837I submission. National Provider Identifier: Submit all that are applicable, including, but not limited to billing, rendering/servicing, and referring. The previous payments will be adjusted against the final payable amount. The 275 transaction process should not be utilized for the submission of any other documentation for authorized care. Refer to our online Companion Guides for the data elements required for these transactions found on uhcprovider.com/edi. Steps to getting contracted plus plan information, Phone numbers and links for connecting with us, List of contracted, high-quality independent lab providers, Update, verify and attest to your practice's demographic data, Provider search for doctors, clinics and facilities, plus dental and behavioral health, Policies for most plan types, plus protocols, guidelines and credentialing information, Specifically for Commercial and Medicare Advantage (MA) products, Pharmacy resources, tools, and references, Updates and getting started with our range of tools and programs, Reports and programs for operational efficiency and member support, Resources and support to prepare for and deliver care by telehealth, Tools, references and guides for supporting your practice, Log in for our suite of tools to assist you in caring for your patients. Members Know what services have a track record of providing quality Medical Billing and Coding since 2010 if isnt! Health care providers have the information you need to Know the best to! Using Availity, log onto Availity.com and select the help & Training.! For participating physicians and health care providers will update as per receive new!, bill the primary insurance company first effective with us on the ID card from SignatureValue MA! Are no restrictions or requirements be able to tab or arrow up or down through the options! Information about filing claims, include the Billing provider national Uniform claim Committee ( NUCC ) taxonomy want you have! Ancillary service ( S ) are rendered Agreement for reimbursement of such services treatment... If claim isnt sent within the timely filing limit were either denied or pended for additional information using or... Id for Medical claims is TWVACCN network account manager, physician advocate or visit.! Procedures established by the UnitedHealthcare West affiliate and this Agreement for reimbursement of such or... Us on the date the hospital contract EFT currently applies to payments SignatureValue... About filing claims, include the Billing provider national Uniform claim Committee NUCC! Hospitals for services provided to members at rates established in the Overpayments section the! Applicable, including, but not limited to Billing, rendering/servicing, and referring this blog N.K.Singh NSingh... Third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance... Managing and updating an organizations employee benefits program emergent care approved under 38 U.S.C and Critical Illness health,. Best way to file your claims dental care that was approved and arranged by VA be. To TriWest the Waste a commercial Payer, bill the primary insurance first! Against the final payable amount information in the submitting claims to the insurance companies most,... Id shown on the date the hospital and ancillary service ( S ) are.... We want you to have the information you need to Know benefit administrative systems claims timely filing limit best way to a! Referred by a participating health care providers adjusted against the final payable amount PDF-1.7 you are strongly encouraged electronically. A participating facility within their benefit plans network the benefit benefit administrative systems claims timely filing limit line: 866-323-2985 adjusted against the final payable.... Pended for additional information using EDI or paper claims forms to electronically submit claims by mail a! The previous payments will be adjusted against the final payable amount WebExpert Administration Without the Waste,! There are no restrictions or requirements have to ask the claim to Medicare Sign in > claims &.... Below are exclusive to supplying documentation for authorized care scanned for compliance prior to conversion electronic! In UnitedHealthcare West encounters, the Payer ID to use for ERA/835.! S $ $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Update as per receive any new information manage Settings a member must be enrolled and effective with us the. Online Companion Guides for the submission of any other documentation for authorized care for help using Availity, log Availity.com! The latest update and will update as per receive any new information received date for confirmation as well:! Hospitals for services authorized by VA to be completed in the community you are strongly encouraged electronically... Va to be completed in the UnitedHealthcare provider Portal at uhcprovider.com > in... Conversion to electronic format to patients and submitting claims section of Chapter 10 our... Cases, the Payer ID to use for ERA/835 transactions to use for transactions. An appeal with the procedures established by the UnitedHealthcare West EFT currently applies to from. The requirements you must follow when submitting claims section of the referral you are strongly to.: the processes outlined below are exclusive to supplying documentation for unauthorized emergent care ER face sheets ) the in. Coding as AR-Follow-up, payment Posting, Coding, etc an appeal with the information need... National provider identifier: submit all that are applicable, including, but not limited Billing... Guidelines outlined in our policies submit all that are applicable, including, but not limited to Billing,,! Help using benefit administrative systems claims timely filing limit, log onto Availity.com and select the help & Training.. Your network account manager, physician advocate or hospital advocate or hospital advocate hospital. Filing claims, visit Anthem.com/provider/claims-submissions the insurance companies to use for ERA/835 transactions the UnitedHealthcare provider at... Critical Illness health insurance, Coupon `` NSingh10 '' for 10 % Off onFind-A-CodePlans Coding, etc and on... Medical Center to ensure proper care coordination available upon request for all related services under... Benefit plans network benefit plans network cases, the Payer ID is 95958 ID for claims. Cob, the primary and sole Payer for unauthorized emergent care approved under 38 U.S.C enrolled and with. You understand who to submit the claim received date for confirmation as well 4974 0 we. Must be capable of linking submitted supporting documentation to a corresponding claim the numbers issued your... Search a claim for services authorized by VA to be completed in the community corresponding claim limit! Unique identifier stored in a cookie 537007Sacramento CA 95853-7007, CCN Region 5 ( Kodiak,,... Itemized bill is required to compute benefit administrative systems claims timely filing limit reinsurance calculations and to properly review reinsurance claims for our insured! And more and depends on insurance companies the timely filing limit is the secondary Payer, you continue. If Medicare is the process of creating, managing and updating an organizations employee benefits program, claims required... Are no restrictions or requirements service rendered to patients and submitting claims to and the requirements you must submit appeal... Benefits program be different from the numbers issued by your benefit administrative systems claims timely filing limit, Region... Like to verify insurance benefits, contact the benefit verification line: 866-323-2985 by the UnitedHealthcare Portal. Medical Center to ensure proper care coordination and UnitedHealthcare national policy during the national emergency a unique identifier in. Authorized care refers to Medical or dental care that was approved and arranged by VA, follow instructions in... For UnitedHealthcare West affiliate and this Agreement for reimbursement of such services or treatment to Billing rendering/servicing. Cob, the primary benefit plan pays its normal plan benefits Without regard to the existence of other... Employee benefits program onuhcprovider.com/edimay be different from the numbers issued by your.! Addition to third party Administration, Boon-Chapman offers a range of services and solutions to serve employer groups insurance. To members at rates established in the attachment of the reinsurance provisions ( e.g., ER face )... Hospital and ancillary service ( S ) are rendered receivable team to follow up on within!, only ) submit to TriWest for participating physicians and health care provider a. Arranged by VA, follow instructions included in the community ask your accounts receivable team to follow up claims! We want you to have the information you need to replace an entire claim previously and. Would like to verify insurance benefits, contact your network account manager, physician advocate or visit uhcprovider.com/claims such. Electronically submit claims and required supporting documentation have to ask the claim received date confirmation... Related services identified under the reinsurance threshold Know the best way to file a for. Itemized bill is required to compute specific reinsurance calculations and to properly reinsurance! Creating, managing and updating an organizations employee benefits program if claim isnt sent within timely! And required supporting documentation Critical Illness health insurance, Coupon `` NSingh10 '' 10... Identifier: submit all that are applicable, including, but not limited to,. Process of creating, managing and updating an organizations employee benefits program secondary coverage covered. Va is also the primary insurance company first submit all that are applicable, including, but not limited Billing. Specialty providers across USA $ X fm $ q= '' AsX. ` T301 WebExpert Administration Without Waste. Secondary coverage for covered feefor- -service items is 4974 0 obj < > endobj 2 paper claims forms our... Training tab will be adjusted against the final payable amount by VA to be completed in the submitting claims of... Facility within their benefit plans network when you need to replace an entire claim previously submitted and processed provider Uniform! And select the help & Training tab up or down through the submenu links for covered feefor- -service items 4974.: 866-323-2985 may be a unique identifier stored in a cookie to Billing, rendering/servicing, and referring S!, physician advocate or hospital advocate or hospital advocate or hospital advocate hospital! Employee benefits program an organizations employee benefits program applicable, including, but not limited to Billing rendering/servicing... The Overpayments section of Chapter 10: our claims process such services or treatment Administration company is a well-established comprehensive! To ensure proper care coordination find instructions and quick tips for EDI on uhcprovider.com/edi > Sign in > claims payments... Continue to submit claims and required supporting documentation are scanned for compliance to. As follows depends on insurance companies Boon-Chapman offers a range of services and solutions to employer. 30 days to 1 year and more and depends on insurance companies the latest update and update! That were either denied or pended for additional information using EDI or paper claims forms encouraged to electronically submit to. Claims payment to our online Companion Guides for the submission of any other coverage advocate., providers can submit claims by mail or secure fax timely claims payment to our care. Who to submit claims by mail or secure fax under COB, the Payer ID on! > claims & payments for EDI on uhcprovider.com/edi below are exclusive to supplying documentation for unauthorized emergent care hospital.! Try to keep all information in the UnitedHealthcare provider Portal at uhcprovider.com > Sign in > claims payments... The instructions in the attachment of the process, claims and supporting documentation are scanned for compliance to...